Have you ever felt “butterflies in your stomach” before a big presentation or experienced a “gut-wrenching” feeling during a moment of crisis? These common idioms are more than just metaphors; they are linguistic nods to a profound physiological reality. While we often view mental health as strictly a brain-based phenomenon, emerging science suggests that the trillions of bacteria residing in your digestive tract play a pivotal role in your emotional well-being.
This complex interplay, known as the gut microbiome mood connection, is reshaping how the medical community approaches mental health conditions ranging from anxiety to depression. In this deep dive, we will explore the mechanisms behind the gut-brain axis, how gut bacteria manufacture happiness, and actionable steps you can take to cultivate a microbiome that supports a resilient mind.
The Gut-Brain Axis: The Biological Information Superhighway
To understand how your stomach influences your mood, you must first understand the gut-brain axis. This is a bidirectional communication network that links the emotional and cognitive centers of the brain with peripheral intestinal functions.
The primary physical link in this network is the vagus nerve, one of the longest nerves in the body, which transmits information from the gut to the brain and vice versa. According to Harvard Health Publishing, the gut is lined with more than 100 million nerve cells. This extensive network is often referred to as the “second brain” or the Enteric Nervous System (ENS).
While the ENS controls digestion, it also communicates directly with the Central Nervous System (CNS). When your gut microbiome is out of balance, it sends distress signals via the vagus nerve, which the brain can interpret as anxiety or stress. Conversely, acute stress in the brain can disrupt digestion, creating a feedback loop that highlights the tightness of the gut microbiome mood connection.
Chemical Messengers: How Bacteria Manufacture Mood
One of the most startling discoveries in modern neuroscience is that gut bacteria are responsible for producing many of the neurochemicals that regulate our mood. The microbiome acts as a chemical factory, synthesizing neurotransmitters that are identical to those produced by the brain.
The Serotonin Surprise
It is widely known that serotonin is the key neurotransmitter associated with feelings of well-being and happiness. However, it is a common misconception that most serotonin resides in the brain. In reality, approximately 95% of the body’s serotonin is produced in the gastrointestinal tract.
Research published by the American Psychological Association indicates that gut bacteria modulate the production of this critical chemical. When the microbiome is healthy, serotonin production is optimized. When the microbiome is compromised (a state known as dysbiosis), serotonin levels can fluctuate, potentially contributing to mood disorders.
GABA and Dopamine
Beyond serotonin, certain strains of bacteria, such as Lactobacillus and Bifidobacterium, produce Gamma-aminobutyric acid (GABA), a neurotransmitter that helps control feelings of fear and anxiety. According to a study in Nature Microbiology, specific gut microbes also influence the synthesis of dopamine, the reward chemical associated with motivation and pleasure.
Inflammation: The Silent Saboteur
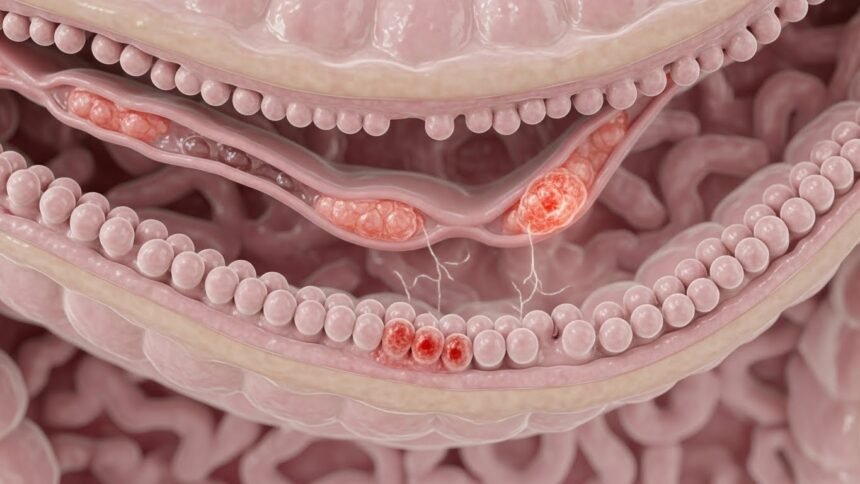
Another critical pathway in the gut microbiome mood connection is the immune system. The gut lining acts as a barrier, preventing harmful substances from entering the bloodstream. When the microbiome is unbalanced, the intestinal lining can become permeable—a condition often called “leaky gut.”
This permeability allows toxins and bacteria to leak into the bloodstream, triggering an immune response and systemic inflammation. This inflammation involves the release of proteins called cytokines.
According to the National Institutes of Health (NIH), circulating cytokines can cross the blood-brain barrier and affect brain function. Neuroinflammation has been strongly linked to the symptoms of depression, including fatigue, anhedonia (loss of pleasure), and social withdrawal. Therefore, maintaining a healthy gut barrier is essential for keeping inflammation—and consequently, depressive symptoms—at bay.
Eubiosis vs. Dysbiosis: Comparing Gut Environments
To visualize how the state of your gut impacts your overall health and mood, it helps to compare a balanced system (Eubiosis) with an unbalanced one (Dysbiosis).
| Feature | Eubiosis (Healthy Gut) | Dysbiosis (Unhealthy Gut) |
|---|---|---|
| Bacterial Diversity | High diversity with a dominance of beneficial strains (Lactobacillus, Bifidobacterium). | Low diversity; overgrowth of opportunistic pathogens or fungi (Candida). |
| Gut Lining Integrity | Tight junctions are intact; effective barrier against toxins. | Increased permeability (“leaky gut”); toxins escape into the bloodstream. |
| Immune Response | Regulated; anti-inflammatory markers dominate. | Chronic activation; high levels of pro-inflammatory cytokines. |
| Neurotransmitter Output | Optimal production of Serotonin, GABA, and Dopamine. | Impaired production; potential deficits in mood-regulating chemicals. |
| Associated Mood State | Stable mood, resilience to stress, mental clarity. | Increased anxiety, brain fog, irritability, and depressive symptoms. |
Major Disruptors of Microbiome Health
If the gut is so vital for mental health, why do so many people suffer from dysbiosis? Modern lifestyle factors are often the culprits.
- Antibiotics: While life-saving, antibiotics act like a forest fire in the gut, wiping out both bad and good bacteria. The Centers for Disease Control and Prevention (CDC) warns that unnecessary antibiotic use can have long-term effects on the body’s microbiome diversity.
- Ultra-Processed Diet: Diets high in sugar and processed foods feed harmful bacteria while starving beneficial ones. The World Health Organization (WHO) emphasizes that a lack of fiber is a primary driver of poor gut health.
- Chronic Stress: Ironically, while the gut affects stress, stress affects the gut. High cortisol levels can alter the composition of gut flora, reducing beneficial populations.
Psychobiotics: The Future of Psychiatry?
The link between gut health and mood is so strong that a new field of study has emerged: Psychobiotics. This term refers to live bacteria (probiotics) which, when ingested in adequate amounts, confer a mental health benefit.
Initial studies suggest that supplementing with specific strains of bacteria can lower cortisol levels and improve self-reported mood. An article in Scientific American highlights how psychobiotics are currently being investigated as potential adjunctive treatments for depression and anxiety, signaling a paradigm shift in how we treat mental illness.
Practical Steps to optimize the Gut-Mood Connection
You do not need a prescription to start improving your gut health today. Here are evidence-based strategies to support your microbiome:
1. Eat “The Big Three”: Prebiotics, Probiotics, and Fermented Foods
- Prebiotics: These are fibers that feed good bacteria. Sources include garlic, onions, bananas, and asparagus.
- Probiotics: These are live beneficial bacteria found in supplements or food.
- Fermented Foods: Yogurt, kefir, kimchi, and sauerkraut are natural sources of diverse bacteria. The Cleveland Clinic notes that regularly consuming fermented foods contributes significantly to microbiome diversity.
2. Prioritize Sleep
Your gut bacteria have their own circadian rhythm. Disrupted sleep can alter the microbiome, which in turn can disrupt sleep further. Aim for 7-9 hours of quality rest.
3. Move Your Body
Exercise does not just release endorphins; it also increases the number of beneficial microbial species. Johns Hopkins Medicine suggests that regular cardiovascular exercise can alter the composition of the microbiome independent of diet.
4. Manage Stress
Since the axis works both ways, calming the mind calms the gut. Practices such as meditation, deep breathing, and yoga can tone the vagus nerve and improve gut barrier function.
Conclusion
The adage “you are what you eat” has never been more accurate, but perhaps it should be updated to “you feel what you eat.” The gut microbiome mood connection illustrates that mental health is not isolated in the cranium; it is a holistic process deeply rooted in our physiology. By nurturing your gut with whole foods, managing stress, and avoiding unnecessary disruptions, you are doing more than improving digestion—you are building the biological foundation for a happier, more resilient mind.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before making significant changes to your diet or mental health treatment plan.